My MP thinks that my life is not good value for money for the taxpayer.
On the 11th of July, NHS England announced which treatments and services it will make available to patients. There were over one hundred policies considered, and twelve of them were "cost-neutral or cost-saving" and therefore confirmed. Twenty two more policies were split into levels 1-5, level 1 being the cheapest and of greatest clinical benefit, and level 5 being the most expensive and of lowest clinical benefit. There is enough money to pay for the treatments in levels 1-4, although that may change now a judge has ruled that the NHS can pay for PrEP. Level 2 includes more treatments for Graft vs. Host Disease, which is excellent news. It also includes penile prostheses for erectile dysfunction. No offence to the people who need this, but it hardly seems quite as important as saving someone's life. Level 4 includes stem cell transplants for people with Lymphoplasmacytic Lymphoma. It's expensive, but not so much that it isn't worth the money.
In Level 5 is "second allogeneic haematopoietic stem cell transplant for relapsed disease". This decision was based on this public consultation, and I have a lot of issues with it.
The epidemiology and needs assessment uses evidence from one hospital in the USA from 1989 and 1998. Data from one hospital, between eighteen and twenty seven years ago. So we're not taking into account any advances in science or understanding since 1998. This seems purposely ignorant considering the NHS had been providing second transplants routinely up until 2013 and has information on all the patients they were provided to. We know how long patients in this country using the methods that are standard are surviving having had second stem cell transplants, yet this is being completely ignored. I can't quite understand why.
They say there is enough evidence to give second transplants to a few, very special people that will somehow be chosen through an exclusive selection process. This sufficient amount of evidence is very limited (an oxymoron, surely?) and rather poor, but they have no intention of trying to obtain more evidence by actually giving more people the treatment that could save their lives and turning second transplants back into a routinely funded policy.
I have tried to simplify the evidence review summary:
Do transplants work?
There is very little published evidence, and the evidence that exists comes from a couple of studies over a period of more than twenty years. The evidence might be biased, and the people involved in these treatments are so varied, there are so few constants that the results are not what one would call reliable, so the outcomes fluctuate. It is clear from the evidence that they do work, but sometimes people die and there are a myriad of reasons for that.
Are they cost effective?
We found one study that recorded the cost of second transplants, but not the cost effectiveness. In short: we don't know.
Could we determine some criteria to decide who deserves a chance to live?
It seems so. If they relapse after a year, that would be good. Being under forty would also help. If the person's relapse is caught early, that might be favourable, and if they had full-body radiotherapy.
(I would fulfil two of these criteria: being under forty and having my relapse caught very early. But seeing as it was only four months after my first transplant and radiotherapy wasn't part of my treatment the first time, I'd be sent home to die.)
When the panel reviewed data from the British Society for Blood and Marrow Transplantation (BSBMT) database for the period 2007-2012, they found that survival outcomes for allogeneic transplants using matched unrelated donors are nearly as good as those using sibling donors; five year overall survival of 30% is comparable with the outcomes of first transplant for some subgroups of acute leukaemia.
If this is the case, why are second transplants considered such poor value for money when they have almost the same outcome as transplants using the best kind of donors, which are routinely funded?
The final decision was that patients whose first stem cell transplant results in relapse should be offered a second transplant if they were in complete remission before the relapse, the relapse is at least twelve months after the first transplant, and they are deemed clinically fit to undergo the transplant by a team of specialist doctors and nurses. However, if a patient relapses within a year of the first transplant, they should not be offered a second transplant.
This is appalling. I am greatly upset by it, as I relapsed only four months after my first transplant. My first transplant came from my sister, who was a 100% match. However, I did not get any Graft vs. Host Disease, which is defined in the consultation as such:
"Graft-versus-host disease is a common complication following an Allogeneic tissue transplant where white blood cells (immune cells) in the tissue (the graft) recognise the recipient host as "foreign". The transplanted white blood cells then attack the host's body cells. Graft-versus-leukaemia response is the desired effect following Allo-HSCT where donor cells eliminate malignant cells."
Essentially, a bit of donor/recipient cell fighting is desirable, because any lurking malignant cells are also destroyed. I had none of this with my first transplant, because my sister was almost too good of a match. I was so lucky to have my only sibling be a match when those odds are just one in four, yet so unlucky as to have that be the thing that came back to bite me. And that would be the reasoning that the NHS would now use when I would be informed that treating me would not be good value for money for the taxpayer. I would be offered chemotherapy to try to keep the cancer at bay, and/or palliative care should I wish to just die as comfortably as possible, the costs of which can amount to equal those of a transplant itself.
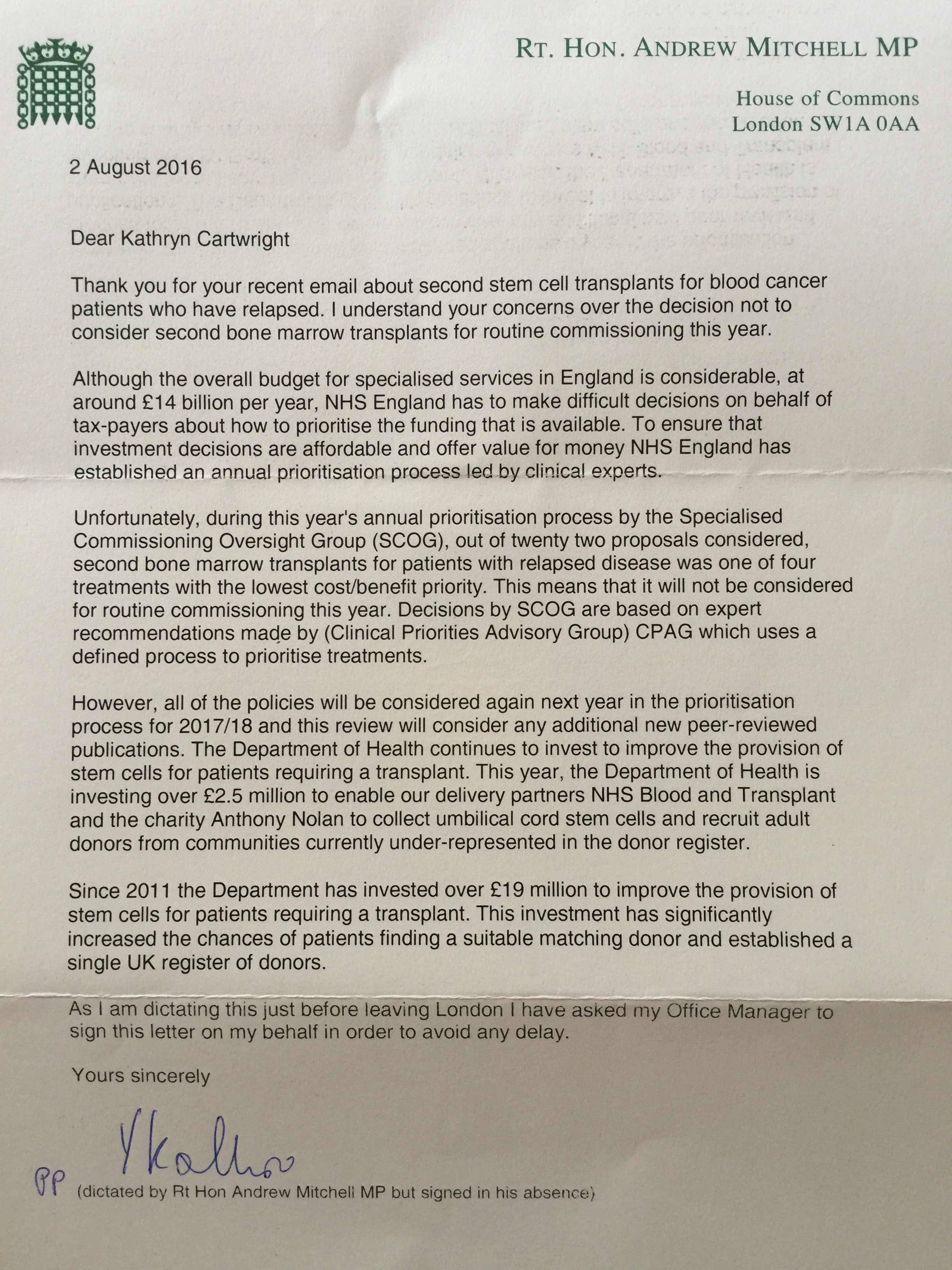
Today I received a letter from my MP, Andrew Mitchell, in response to an email I sent via Anthony Nolan's campaign to ask MPs to support funding for second transplants. He was not particularly interested in doing so. He has met me, and I reiterated this and my story in my email, yet he still decided to write back and say that actually, treating me has been very poor value for money and basically, the NHS should not have bothered giving me the past eight years.
He also felt the need to inform me of just how great the government have been at investing in improving the provision for stem cells for patients who need a transplant. We appreciate that, but it seems somewhat redundant when that provision is not allowed to be used for certain people whose lives could be saved just because their disease came back earlier than someone else's. It seems barbaric to me to decide that these people are not "cost-effective". I think it is the terminology that bothers me, like they have gone out of their way to try to forget that these are real people that this decision will affect. Human beings with parents, siblings, children who simply experience bad timing and for that, they are written off as unworthy of help. People who may have worked a long time, paying taxes, expecting the NHS that they have put money into to help them in their time of need, being told that that money is going to pay for a prosthetic penis instead of a treatment that has a good chance of saving their life. Or people like me, who get an aggressive cancer at sixteen and never have a chance to work but grew up believing that as a wealthy first-world country, our healthcare system was there to treat the sick and will now be informed that actually, no, it's not for everyone. Not if you're not "cost-effective".