The 2nd & 3rd; I have a pneumothorax!
The 2nd of March. I woke up this morning and it was clear that I needed to be in hospital. I had to have the oxygen on 3 litres when at rest which is far from acceptable. We talked about what was the best plan - do we ring haematology? Email Dr. Thompson? Or just go to A&E? We came to the conclusion that it was best to ring the CNS team, who got back to us very quickly and said to come up to the ward immediately. I finished my coffee, Mommy packed a bag and in we came.
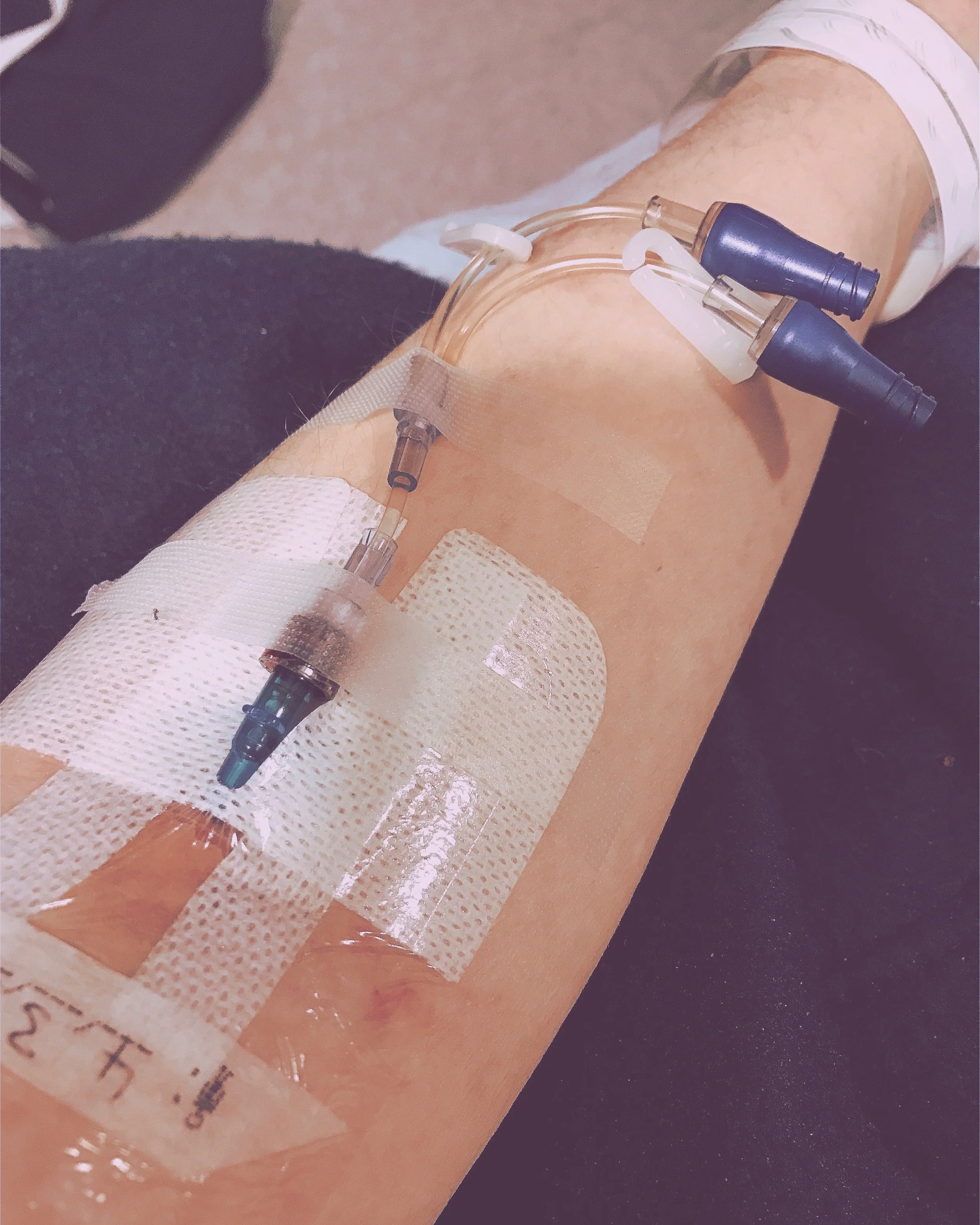
Jo, a nurse who has looked after me before and knows me, came and did my obs, and the first of the many doctors I saw today came. His name was Aran (I don't know how he spells it so I am making an assumption) and we had a chat about my symptoms, then he needed to take some bloods, and for me to take off the oxygen for half an hour so he could do an arterial blood gas to see what the oxygen levels in my blood were like. He had a tough time getting the artery because mine are so small and elusive but he got there. It was not so terrible, but I will bruise.
He then went away, and after a while, he returned with Paul, one of the regs who saw me before Christmas. At rest, my sats were fine, which I found ridiculous but that was what it said. I suggested we do another blood gas after I'd walked a bit, and see what that was like. We had to leave me off the oxygen another hour to do that, so just after half past one, Aran came back with more needles and sent me off on a walk up and down the ward. I had to stop before I got to the end, but I finally got back to him, and felt like I might die. What was worst was that I couldn't put the oxygen on to recover, and I couldn't move or speak, just had to let him jab around in my wrist and after some time, elbow, to get the second gas. The other investigation that needed doing was a chest x-ray, which also happened very speedily. Everything has been so efficient today! So I went down to x-ray with a nurse and we had a nice chat about how we both look young (she said she was 40 which I do not believe) and then we couldn't come back up in the lifts because the fire alarm was going off. Thankfully it was not a proper fire, and we returned to the ward.
Paul and Aran came back with looks of great excitement on their faces, and Paul asked "Have they told you?" Very much not. It appears I have a pneumothorax! That's a collapsed lung, basically. No reason, just another stupid thing that my body has decided to do.
To fix this, Paul had called the respiratory team, and a consultant called Ben Sutton came to see me. His opinion that the best thing to do would be a chest drain, because just aspirating with a syringe might not work and if I went home and it collapsed again we'd be in trouble. I agreed with this, and also mentioned that Dr. Thompson might want to know about this. He then came up to see me, and was not impressed that the ABGs had been done before the chest x-ray. Nevermind!
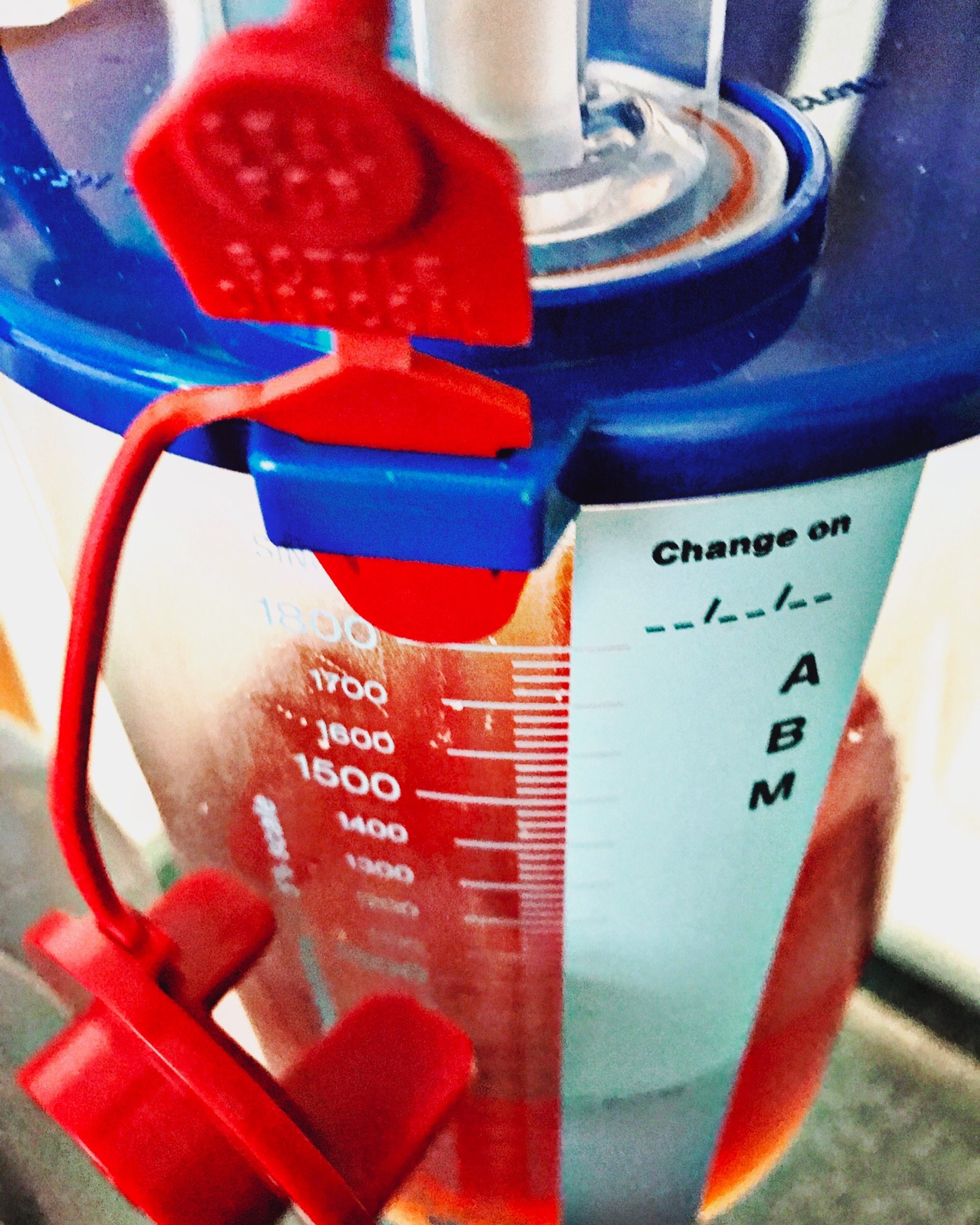
So, chest drain. We had to wait for a respiratory reg to come up to do it, and Dr. Thompson supervised. We went through to a tiny side room, the purpose of which is something I am not entirely sure of, and I sat up on a trolley with a sheet across my front while Dr. Lugg, the reg, gowned up. First, he cleaned me, then poked me a lot between the ribs to find the gap he needed to get the needle in. He stuck a sticker on so he knew where to go back to, then I had lots of local anaesthetic around the site. There was a small cut, then there was a needle, and a wire to guide the doctor, some tubes, and a lot of pushing to get the tube into the place where it needed to be. Then he attached a very large tube, and many bubbles poured out of me. It suddenly made sense that the rumbly sensation I have been feeling was bubbles in my chest, and now they are on their way out. I could see them moving up and down the tube as I inhaled and exhaled.
It doesn't feel great, but I've had worse. The drain is firmly attached to my side, and the movement of air is slower now. I've had another chest x-ray to check the progress, which showed that it's improving but hasn't fully reinflated yet, which is how it feels. Dr. Thompson suspects I will need the rest of the air to be actively suctioned out because it might not all come out on its own. I'm sure that'll be fun. While I was waiting to come back to the ward, I was talking to the nurse who was with me, Craig, and we were comparing physio stories, because he'd had a car crash which resulted in a brain injury and he'd been paralysed on one side, so he had to learn to walk again too. However, he was a very good physio patient unlike me, who would pretend to be asleep.
Mommy didn't really want to leave me, but by half past eight there were no signs of me having a bed, so I told her to go, and shortly after that, I got moved!
Now I am in a cubicle (my favourite way to be) and going to the bathroom with the drain is interesting (I have to buzz someone), but I'm alright. I don't think I will get much sleep tonight - lots of podcasts, maybe some Netflix. I need to plug my chargers in and get my pyjama top on, but I don't need assistance for that. I do hate being so dependent.
The 3rd of March.
I am in NHS limbo. It has been a day of waiting. I did get some sleep - I don't know what time I dropped off but I woke up at 9 in a rather curious position but at least I had some rest. However, that meant I had missed breakfast, so I asked the nurse for some bread and marmalade, and that had to do. It was not dissimilar from what I'd have at home anyway.
I spent my morning wrapping myself up in my blanket and sheets, trying to get warm, and not quite falling asleep. Praveen, the reg from clinic, came to see me, wondering what the hell had happened since then, so I explained, and he had nothing to add so off he went again.
Mommy arrived with food and more clothes, and we essentially sat around all afternoon waiting for my chest CT/Dr. Thompson, whichever came first. It ended up being the scan, and I had the fastest porter in the world (he was even faster than my chair!).
When I returned to the ward, I emailed Dr. Thompson to let him know, and he replied to ask where I was, so I told him and he materialised shortly after. He looked at my bucket of chest fluid (it's delightful) and determined that the lung isn't going to reinflate fully on its own, so I need to go to the respiratory ward where they can use suction to get the last remaining bits of air out. We can't do that up here because there isn't the kit or the expertise within the staff if there are complications, which means that I am stuck until a bed becomes available down there. That was just before 4, and now it is nearly 8.30 and nothing is happening. It is nobody's fault, it is just that the hospital is literally crammed to the rafters with patients and I can't go and have the treatment I need until someone moves out, but they need somewhere to go. Until that happens, I am taking up a haematology bed which could be being used for a patient who needs it, and it will take longer for me to be discharged than it would have if there were enough spare beds to begin with.
Mommy and Daddy have left after packing up all my things for when I do move, and I am just sitting on my bed, watching tv on my iPad and looking up hopefully every time someone walks past my room. If I think about how shitty this situation is, I nearly start to cry, but if I do that, I won't be able to breathe at all.